By Claire Martin, 2nd July 2024
I have observed more than sixty Court of Protection remote hearings (via MS Teams or Cloud Video Platform) but only one hearing in person, at a regional court (Newcastle). There were real challenges with that one – such as no listing of the hearing on the noticeboards at the court and no court staff to assist. So, I was excited and also a little bit nervous to be going to Teesside Combined Court in Middlesbrough to watch a whole day hearing.
I am delighted to be able to report what a positive experience it was, as a public observer, and would highly recommend in-person observations if they could all be like this one.
In this blog I won’t be reporting on the substantive issues of the hearing but on the process and experience of accessing the court in Middlesbrough as a public observer in the Court of Protection.
Background
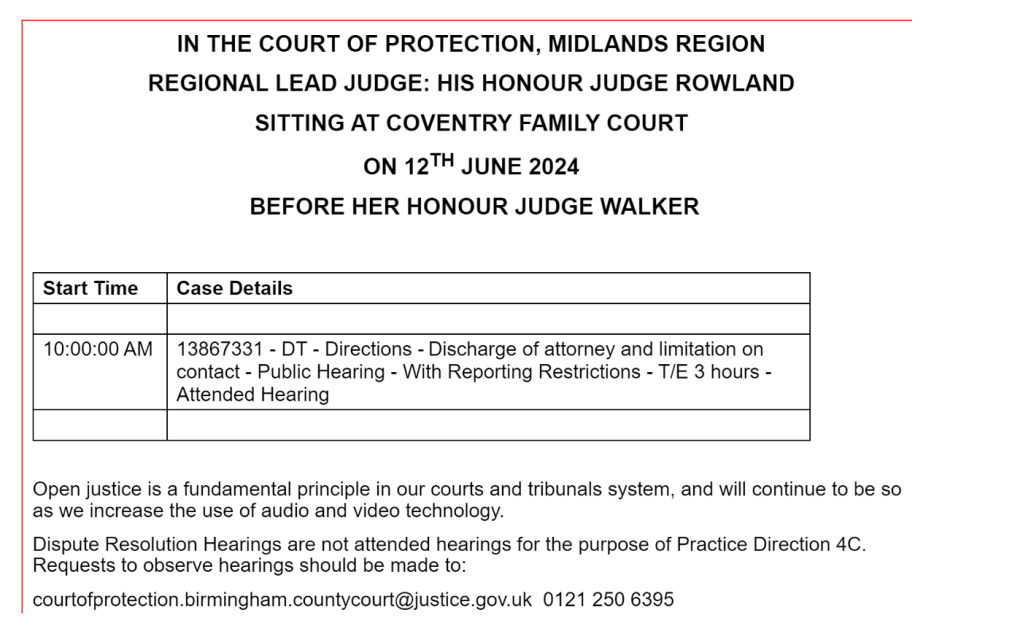
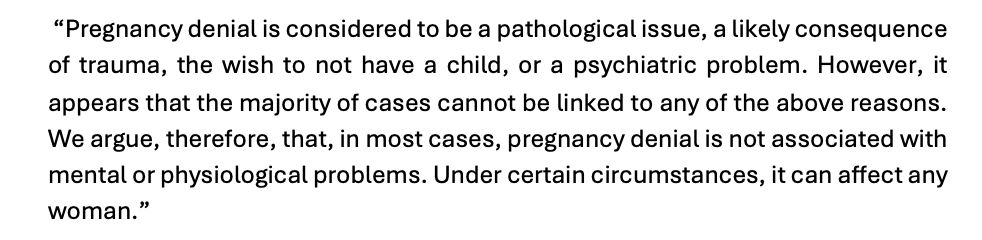
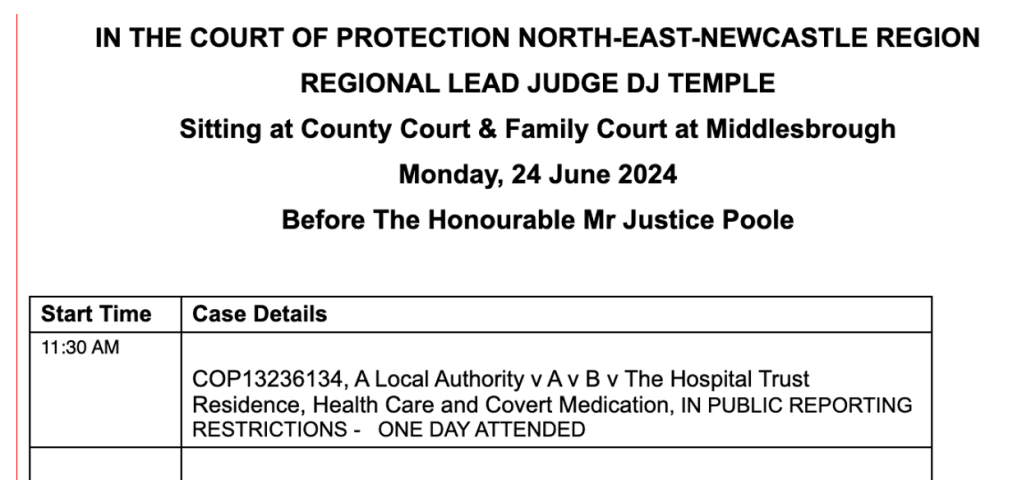
A case we’ve been following for a long time before Mr Justice Poole (COP 13236134) was listed for 11.30am, Monday 24th June 2024, in person at Teesside. Here’s how it was listed – as “ATTENDED” (i.e. in-person) – when the lists were published on the Friday before.
I hoped to observe remotely, so I emailed the court to ask whether it might be possible to set up a link, but by this time it was Friday evening and I was concerned that the court staff might not read my email in time and I might miss the hearing. I was observing with a clinical psychology trainee, Amy (who will be writing her own blog about the experience), and we liaised about what to do over the weekend.
Given a history of staff (across different courts) not sending out links in time, we decided, since we live in the North-East, to drive to the court together to observe in person. I emailed the court staff again on the Sunday night to let them know we would be coming along in person, so as not to put them to the trouble of setting up a link if we were the only people who’d asked for one.
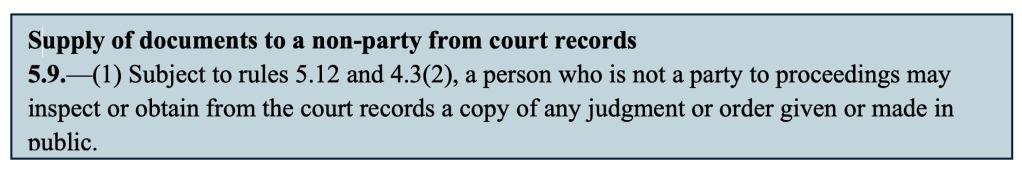
As it happened, the court staff were very responsive, emailing back at 10.10am on the Monday morning, informing me that a remote link could be set up (and indeed they had received another request for a remote link, which they set up for that person). They sent the Transparency Order at the same time (the injunction which informs us what we cannot report about the hearing – usually the identity of P, the protected party, anyone connected to them such as family members, or any information that is likely to enable their identification). It’s important we receive this document in writing before a hearing so that we understand and do not breach the court’s reporting restrictions.
I was pleased that we had decided to go along in person: if a link hadn’t been available, we wouldn’t have had time to make that decision, and get there in time for the start of the hearing.
It was a very, very hot day. We made sure we left in plenty of time to get to Middlesbrough, find somewhere to park, walk to the court and get through security. We built in a lot of contingency time in case of delays.
Finding the court
We were a little bit flummoxed working out which court we were visiting. The listing said: ‘County Court and Family Court in Middlesbrough’ but didn’t give an address. When we put the court name into Google Maps, what came up is ‘Teesside Combined Court Centre, Russell St, Middlesbrough TS1 2AE’. As the court listing does not have a full address or postcode, we wondered whether there were two courts and whether we would be walking to the correct one. Newcastle has two courts – Newcastle Quayside Law Courts and Civil Family and Tribunal Courts – at opposite ends of the city a long walk from each other.
The Court of Protection sits under the Family Court, so I thought that the ‘Combined Court Centre’ might not be the correct place. There were two other courts in Middlesbrough – Teesside Magistrates court (I knew it wouldn’t be that one), and Teesside Justice Centre, which (on Google Maps) is listed as ‘Family Court’. What to do? We decided to go with Teesside Combined Court Centre because that’s what came up when we put the words from the listing (County Court and Family Court, Middlesbrough) into Google Maps. Luckily we had made the right call.
It can be confusing knowing where to go when you are not part of the court system – I wonder whether people who need to attend courts for their own hearings experience the same uncertainty we did.
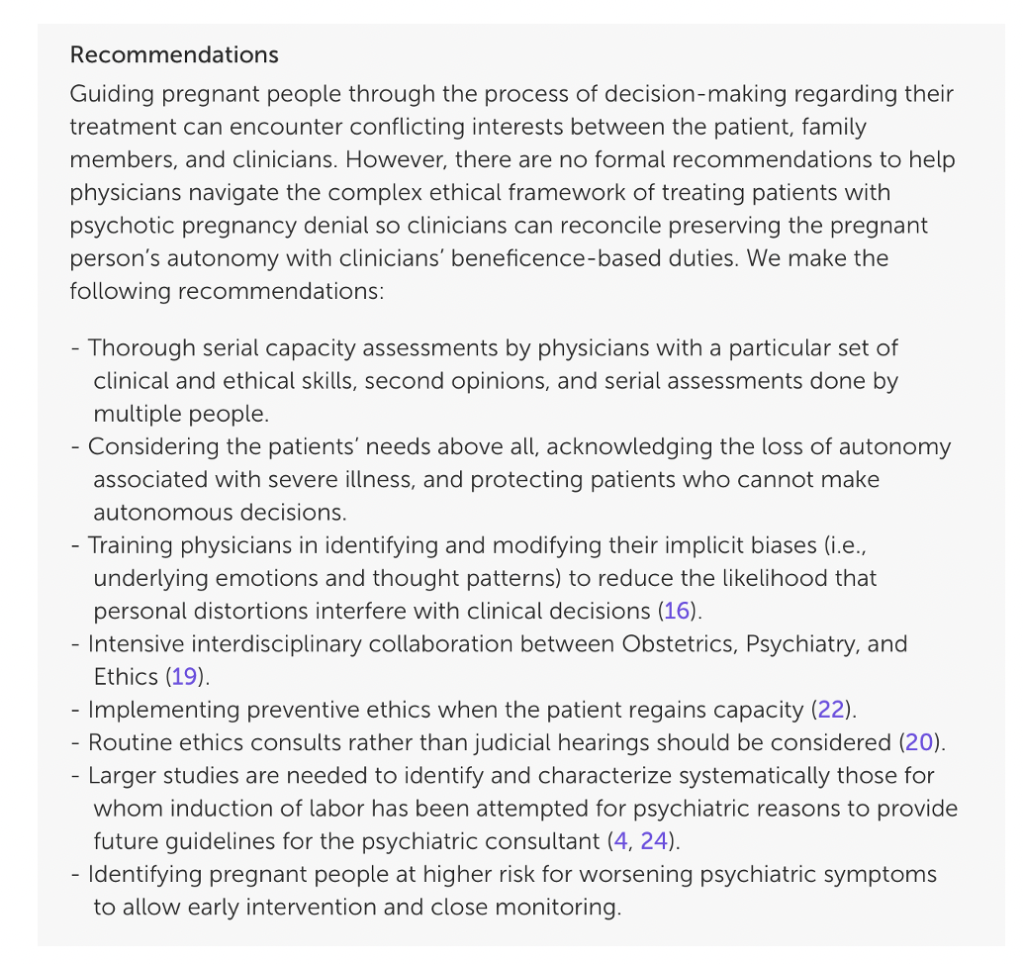
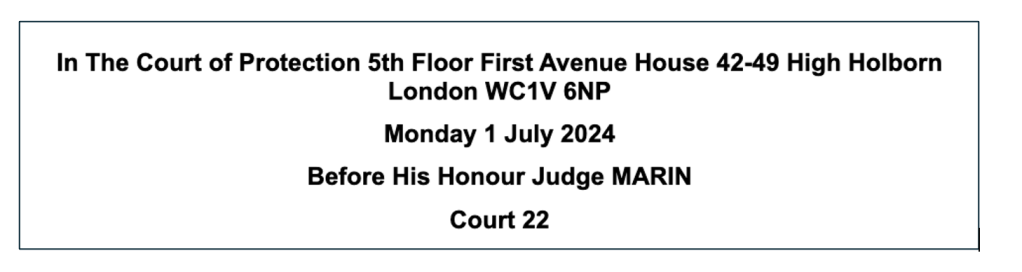
A simple solution would be to list the full address and postcode of the court. Some listings do this (such as Court of Protection hearings at First Avenue House in London), see for example the listing below for a hearing on 1st July.
I had a quick look at all Court of Protection hearings on CourtServe for July 1st 2024 and found that there are several listing inconsistencies: some have place name only, some court name only (the most common) and some have full address including postcode.
Table 1: CourtServe Listings for the Court of Protection for July 1st 2024
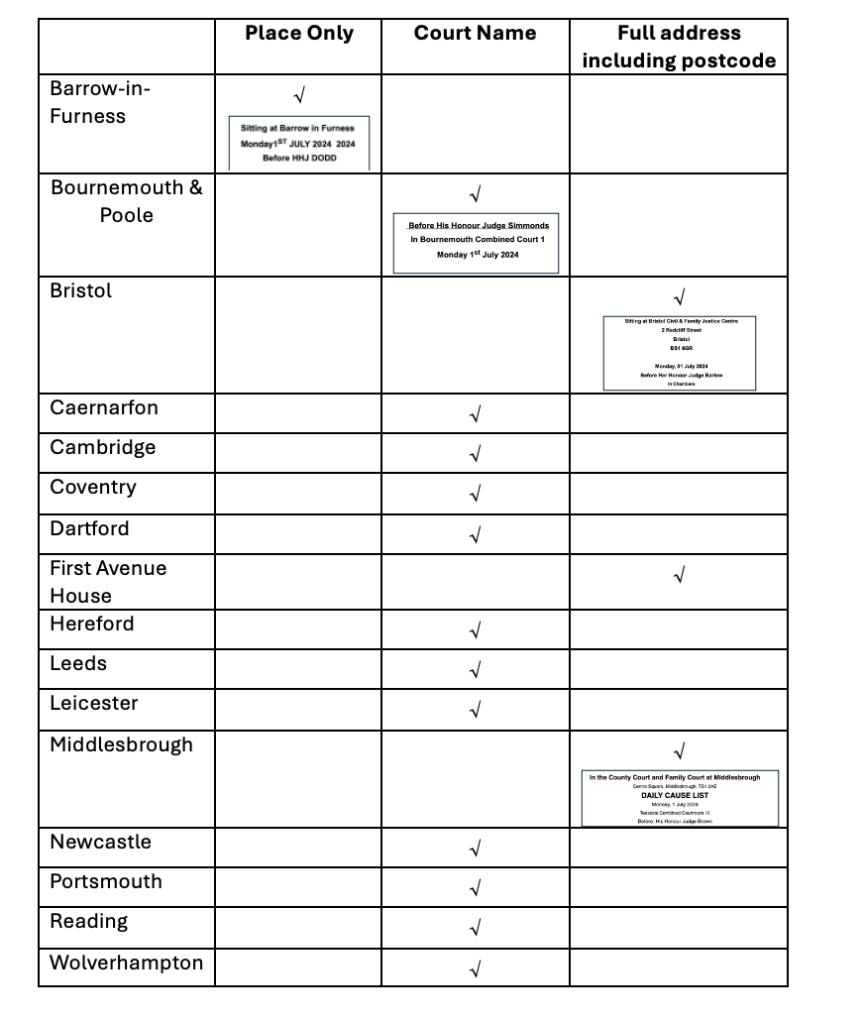
Middlesbrough now had the full address and postcode for 1st July! Very helpful when there are three courts in the city and Google Maps comes up with confusing instructions.
I’ve learnt subsequently that I could have used “Court Finder” to get this information – but I didn’t know about that at the time, and I’m guessing lots of other people don’t either.
A really good experience of open justice in person
Here are the ingredients that made this such a good experience.
Efficient and polite security
When we arrived at the court there was a table to place bags on for searching. The security guards were very respectful and polite, asking us to remove items rather than rooting around in our bags. We needed to show the keyboards of our laptops and then pass through the security scanner ourselves. The guards used a scanning wand to ‘frisk’ us and this was done efficiently and comfortably. Any ‘offending’ items had to be handed in and collected after the hearing. I still had my brush with mirror (glass) and tweezers and perfume (glass) which I should have remembered to leave at home after the last in-person hearing I went to! It didn’t matter as the staff were very personable, popped them in a bag, gave me a ticket and it was all dealt with speedily and professionally.
This is in stark contrast to some recent reports of over-zealous court security and inappropriate, sexualised language and touching as part of entry searches in different courts (see here and here).
Accurate listing
As soon as we were through security, we saw on the left-hand side there was a noticeboard with the court’s hearings for that day. One of the security guards asked which hearing we wanted, and we mentioned Mr Justice Poole. The hearing was there on the board, with the courtroom number. the guard said he wasn’t sure it was public, and we showed him the listing on the board which said ‘public’. Then he told us which floor the courtroom was on and we made our way there.
This contrasts with the other in-person I have attended in Newcastle (and blogged about here) when the noticeboard did not have the hearing displayed and we couldn’t find court staff to help us to find out where the case was being heard.
Helpdesk
The hearing we were observing was on the second floor of the building. There was a helpdesk as we went into the main court room circular corridor, with two people ready to assist. They were very helpful. Again, they said that Court 4 was ‘usually for the Family Court’ and wasn’t likely to be public. I explained that it was a Court of Protection hearing and was listed as public, and that I had observed this same case before, remotely. She was very happy to take us along to the court and, given that we didn’t know the etiquette and how to alert the court usher that we were there, the person from the helpdesk went into Court 4 for us to find the court usher, Olivia, and tell her we were there. She made it seamless, which was much appreciated because we didn’t want to walk into the courtroom when we were not meant to, but equally didn’t want to miss the hearing. Olivia came out of the court and took our names and told us when to come back, and that all parties would be waiting outside, and we could enter with them.
Again, this contrasts with my experience on the day in Newcastle where there were no staff to ask for help – that could have just been that day, or perhaps they were elsewhere dealing with other matters, but I didn’t notice a helpdesk in the style that Middlesbrough had one. It’s a very good idea – I saw the helpdesk staff assisting lots of people (who seemed to be looking for the court for their own hearings), not only to locate the right court, but also explaining to them what to expect in terms of when things started and where to sit and wait.
Courtroom Seating which meant we could see and hear proceedings
On entering the court room, we saw Olivia sitting in front of (and lower than) the judge’s bench, at her own ‘bench’ ready to administrate proceedings. We entered to the side of the courtroom and, given that we had met her already, and she knew who we were, I asked her where to sit and she indicated the side benches. This turned out to be a very good perspective because we could see the faces of counsel and the judge (unlike in Newcastle where you sit at the back and can’t see – or often hear – counsel, because they face the judge). Being able to see everyone’s face also meant we were better able to hear what everyone was saying.
Another public observer, Tim Sugden, blogged about his experience, noting that, when sitting at the back of a court, “what counsel in the front row said was difficult to hear”. He made the important point: “It’s not open justice if you can’t hear what is being said in the courtroom. My experience is that this is a recurrent problem in magistrates’ courts – and now I’ve found the same problem in the Court of Protection as well.” I have also observed remote hearings which were very difficult to follow because the sound quality was so poor. Celia Kitzinger has blogged about a remote hearing that had no sound at all – and even though there were several people (not all observers, she didn’t think) on the remote link, and she alerted the court staff to the problem, the hearing went ahead regardless!
Hybrid hearings (that are part in-person and part remote) can be particularly challenging, depending upon how sophisticated the court sound system is. Even when there are microphones for each person who is going to be addressing the judge (and for the judge themself) people do not sit still (understandably!) and when they move about, and especially stand up, the microphone does not go with them. At a hybrid hearing at the Royal Courts of Justice, Gill Loomes-Quinn commented in her blog contribution (here) that “the sound quality via the remote link was suboptimal”. Gill struggled to hear witness evidence from a nurse in the case, and this was at the Royal Courts of Justice, where I would expect the sound technology to be good. Sometimes it’s not only public observers who cannot hear, as Tom McBride described, in this evocative piece describing the Royal Courts of Justice hearing in the same blog:
“The screen, split up into three different video feeds (showing the witness box, the judge’s chair, and the remainder of the courtroom), gradually becomes busier as barristers, witnesses, observers and staff enter through a door in the corner of my screen. I hear bits and pieces of hushed audio through microphones set up in the courtroom, though nothing is clearly audible. Initially, I assume this is because the remainder of the microphones are yet to be turned on; later, I learn that it is in fact only this microphone which works, which becomes apparent to me when a barrister asks a witness to speak more loudly so that her audio can be picked up.”
I teach at a university from time to time – they have small, attachable microphones with a clip-on control box, that we are asked to wear so that when we move about the sound quality is not diminished for the audience. They are rechargeable and sit in docking stations. This would be a good solution.
No inaccurate prohibitions on electronic devices
There was no problem taking in our laptops and mobile phones (although mobile phones, understandably, had to be switched off or on silent). And there were plug sockets to plug our laptops in. There was someone sitting in front of us, also typing notes on a laptop – I think she was a junior lawyer, because one of the barristers came up to speak to her at the lunch break.
This positive experience contrasts with the confusing and incorrect advice in a report by HMCTS recently published (and later updated in May 2024) about public access to the courts, stipulating that laptops and other text-based electronic devices could not be used in courts. This letter, from the Courts and Tribunals Observers’ Network, challenged the report as follows:
“A prohibition on the use of laptops and other text-based devices (para 3.6 of the Guide) in conflict with their permitted use under the Criminal Practice Directions for the purpose of taking notes “by silent electronic means” and as borne out by our daily experience as court observers. (Until recently, 6D.1 of the Criminal Practice Directions expressly permitted notes to be taken using “silent electronic means” while the new Criminal Practice Directions 2023 is silent on the issue. The Guide was updated on 9 February 2024 to permit the use of laptops for typing notes, but this still ignores the common use of laptops to send and receive information about the case during the hearings by email correspondence with court staff and legal representatives).”
The Network reported that the Lady Chief Justice responded to the letter, acknowledging “that the HMCTS advice wrongly suggested that laptops could not be used in court and noted that the service had taken steps to make the necessary correction”.
However, despite the correction, some courts continue to prevent people from using their electronic devices – see Peter Bell’s recent experience in a Magistrates’ Court in Weymouth: “I am looking on my mobile phone to find the listing to try and locate the name of the Defendant and the case reference when the Legal Advisor barks across the well of the Court at me – is that a mobile phone? I hold it up and say, I am trying to look at the hearing list …I am told that I must switch off any mobile phone when I come in to Court (see later for my comments on this). I do as I am told – he is much bigger than me! – and switch off my phone.”
Observers were treated as a routine in court proceedings
When proceedings were underway, the judge noted at the start that observers were present and checked with counsel that we had been sent the Transparency Order. We did not have a sense that we were unwelcome aliens, a threat to the court, or a risk-management issue. These sorts of unsettling experiences have been described by some other observers
In this blog about a hearing before HHJ Burrows, Celia Kitzinger describes how she and another observer tried, and failed, to attend the hearing because the decision not to provide a link (why not?) was made too late.
“Had we known earlier that the hearing could only be observed in person, one of us might have made the 1-2 hour journey to Preston to observe it. But the judicial decision not to provide links to this hearing was conveyed to us way too late to make this possible – and this must surely have been evident to the judge if he’d given it a moment’s thought. […] Of course, sometimes it’s simply not possible, especially in regional courts, to provide video-access to fully in-person hearings because courtrooms aren’t supplied with the appropriate equipment or there are no staff available to set it up. Requests for remote access can impose intolerable burdens on the court or its staff. But in this case, the non-availability of a video-link was attributed not to resource problems but to a judicial decision simply not to provide it.”
On another occasion, Amanda Hill received no response from the court, either by email by telephone, and when she did get to speak to someone, the hearing had finished. She was simply told “sorry for any inconvenience caused”. And in this blog, George Palmer, a law student, was refused entry despite having sent requests in plenty of time (and another observer being admitted to the remote hearing): “Disappointed, I was left unable to join the hearing, without a sufficient explanation by the court as to why my emails were not passed across to the judge.”
So, all in all, given the variety of experiences of observers of different courts and judges, we’re impressed by our experience in Middlesbrough. We were admitted without fuss, and sat silently observing, without feeling unwelcome or in the way.
Good ongoing communication
We were kept informed (again by Olivia) when the break after the morning session turned into a full lunch break (which was not the initial plan). We were sitting in the corridor waiting for the hearing to resume but a decision had been made to have a lunch break and she came to let us know. She must have had lots of other jobs to do but she kept us in mind.
An on-site café
There is an on-site café at Middlesbrough court, which made things much easier. If you leave the court building for any reason you must go through security again. We did, in fact, opt to do that after eating lunch because it was hot in the building – and getting back in through security was as efficient as the first time. But the cafe meant that if time had been tight, we could have stayed on site. Many courts don’t have this – the answer is to take a packed lunch and some snacks (and a bottle of water).
Final Observations
Observing in person means not being able to wear your slippers and change your clothes if you are too hot or too cold. It was an exceptionally hot day, and the court building had no air conditioning, or fans in the courtroom. I had dressed for the weather but I will always make sure to have layers in future in case the room is air conditioned (do UK courts have this facility?) or in case it gets too hot. As observers on this occasion, we were actually closest to the open windows in the courtroom, with a gentle breeze wafting in. They had to be closed at one point due to building noise outside, and I immediately started to feel hot and sticky. I very much felt for counsel who were wearing their wigs and weren’t seated near the windows. The swelteringness of it!
Being an in-person observer, watching how a remote observer is admitted and responded to, meant that we could see how the court usher made sure the remote observer had true access to the hearing. I don’t know what the experience was on the other end, but before the hearing was underway, the usher checked that the observer could see the court and hear. At first there was a glitch in joining and the usher patiently dealt with this. I have had several experiences as a remote observer checking I could hear – when the usher is speaking, often sitting in front of a microphone. What then happens in the hearing is that counsel (in particular, although judges do this too when they are shifting their attention between screens and witnesses for example) stand up to address the judge. This means that they move away from their microphone and often become inaudible. This must have happened on this occasion because at one point the usher asked Katie Gollop KC to reposition her desktop microphone because the remote observer could not hear her. I assume the observer emailed the usher and was responded to straight away. Another exemplary aspect of this hearing, for open justice. I have recently observed a different (remote) hearing in Norwich, however, where there was one microphone shared between all counsel – the usher had to scurry about the courtroom switching it between people as they addressed the judge.
A final observation is about the compassion I witnessed the judge show to the mother of P (the protected party). She was in court for the hearing (which was about plans to return her adult daughter to live with her – after five unhappy years in a residential care home). At the start of the hearing P’s mother sat alone behind all counsel (who are on the front bench facing the judge) and their solicitors and junior counsel who sit on the row behind them. She was behind a pane of glass and in what turned out to be the dock. I thought that quite ironic, because the way she has been characterised by the Local Authority and NHS Trust certainly positions her as the culprit in these very sad proceedings. I don’t know whether she knew she was in the dock, and her own legal team had not directed her elsewhere. However, when Poole J entered the court room he said, kindly: “You are sitting in the dock! Is there somewhere else you can sit?”
P’s mother laughed diffidently and moved to the side of the court, directed by (I think) her legal team, sitting beside them for the remainder of the hearing. Whatever her role in her daughter’s life, it must have been very hard for her on her own in this intimidating courtroom, hearing counsel unanimously blame her for what has happened. I hope she could hold in mind the small gesture that Poole J showed to her at the start of the hearing.
We will blog about what happened in the hearing soon.
Claire Martin is a Consultant Clinical Psychologist, Cumbria, Northumberland, Tyne and Wear NHS Foundation Trust, Older People’s Clinical Psychology Department, Gateshead. She is a member of the core group of the Open Justice Court of Protection Project and has published several blog posts for the Project about hearings she’s observed (e.g. here and here). She tweets @DocCMartin
Photo credit: The copyright on this image is owned by Oliver Dixon and is licensed for reuse under the Creative Commons Attribution-ShareAlike 2.0 license. It’s been slightly cropped for the display here.