By Celia Kitzinger, 4th August 2025
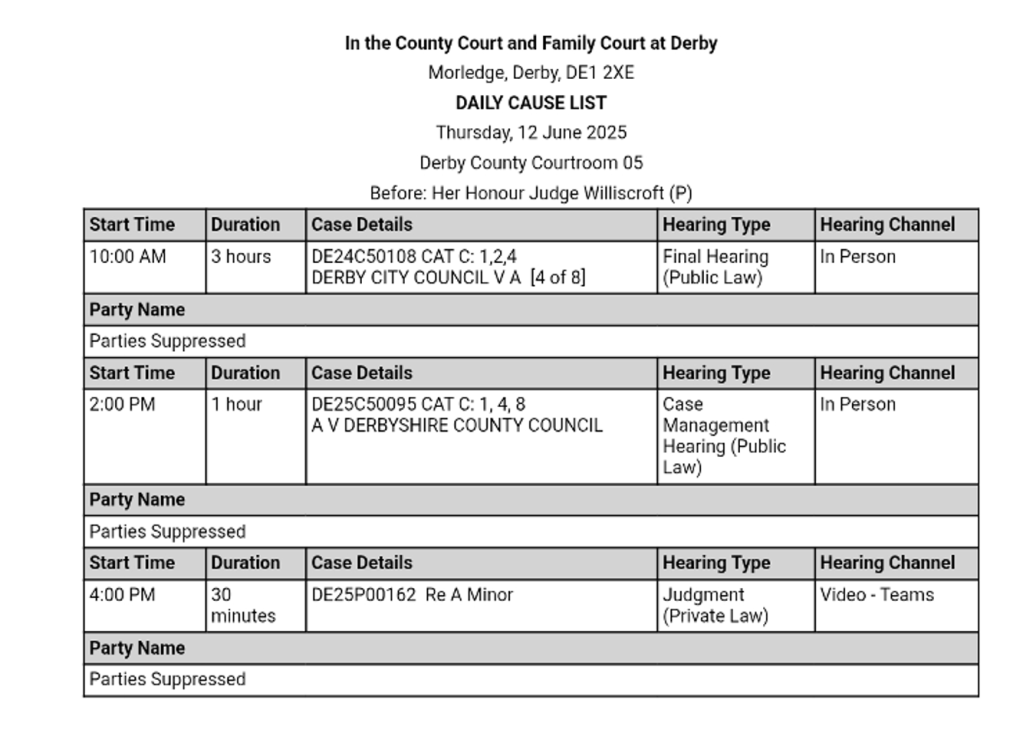
The case, COP 20018026, before Mr Justice Hayden on 22nd and 23rd July 2025, appeared in the Royal Courts of Justice Daily Cause list as concerning “serious medical treatment”[1].
In an opening summary[2], counsel for the applicant explained that the case was about a man in his sixties who’d suffered a significant stroke and had been unconscious on a ventilator in the Intensive Care Unit (ICU) since 12th May 2025 – so more than two months. He was not showing any signs of neurological improvement, and his physical condition has deteriorated.
The clinicians said that very limited support is currently being provided by the ventilator and there is an 80% chance of “success” in withdrawing mechanical ventilation – meaning that the patient would be able to breathe on his own and would survive extubation. Once extubated successfully, he could then to be transferred out of the ICU and could be cared for in a nursing home. If extubation failed, the patient would receive only palliative care: doctors would not return him to mechanical ventilation, or administer a tracheostomy.
The family want ventilation to continue. They believe that he will recover. They say they believe in miracles. According to the clinicians, “extensive and detailed attempts to reach agreement with the family” have failed – and so they’ve brought the case to court.
It seems that this was intended to be a directions hearing – but Mr Justice Hayden, following his well-versed dictum that “delay is inimical to Ps’ best interests”[3] heard it there and then, and made a declaration that it was lawful for the ventilator to be withdrawn.
I’ll describe what happened at the hearing, and what I learnt from the Position Statements, and end with some reflections about the tension between protected parties’ rights not to be given treatment contrary to their wishes (or best interests) on the one hand, and the right to a fair hearing (for everyone) on the other hand.
The hearing
It’s listed as a hybrid hearing and I’m observing it remotely. All the parties are in the physical courtroom: only some family members (they’re not parties) and a medical witness are attending remotely. It’s listed to start at 10.30am, but doesn’t begin until 11:39am (I don’t know why). (NB Quotes purporting to record what was said at the hearing are based on my contemporaneous touch-typed notes – they are as accurate as I can make them but unlikely to be verbatim.)
The applicant NHS Trust is represented by Francesca Gardner (of 39 Essex Chambers). The protected party (“P”) is represented by David Lawson (of Serjeants Inn Chambers) via his litigation friend the Official Solicitor. There are also family members in court: P’s second wife and one son are in court in person, one daughter[4] and P’s brother are together on the video platform and another daughter joined for the second day (also online). It was said that the wife required an interpreter and that the son would take on that role today.
After the opening summary, Mr Justice Hayden – a judge who looks to me to be in his mid-sixties – comments that “80% odds at age 65 are pretty good odds for anything, actually” (it does sound self-referential!). He goes on to say that “It’s a long time since I’ve seen a Position Statement with as little information as this. And I’m the wrong judge for that.” I take this as reference to this judge’s intensely P-focused approach. He then “interrupted” (his word) counsel’s opening speaking slot by turning to P’s son, sitting in the front row with P’s wife, and asking him a series of questions about P (“I’d like to know a bit more about your dad”). This does not elicit a great deal of information: P “liked politics and watching news all the time”, he was clearly a family man “every day he called the rest of the family to find out how everyone is”, he enjoyed cooking but not – Hayden J asked (as always!) – football. Then the judge asked questions directly about the current situation, though P’s son had not been sworn in and was not, at this point, giving witness evidence.
Judge: There’s a good chance he will be able to manage without the ventilator, and that may mean he comes out of hospital into somewhere more private that better promotes his dignity, and closer to your family. The doctors don’t guarantee that, but 80% odds are very good. But that’s not you want.
Son: Yes. I have a strong belief he will come back to life.
Judge: Tell me what you want to happen.
Son: The hospital tell me they have done whatever they can do. They can’t do any more. I have a strong belief he will come back to life.
Judge: So what do you want them to do?
Son: I want them to continue the ventilator – because his pulse, everything, is working. So why they want to remove the ventilator?
Judge: They think it very likely he will survive.
Son: Of course.
Judge: Some would say he deserves that chance.
Son: Yes. My Lord.
Judge: That it’s not in the gift of his children. That he deserves that right – to come off the ventilator, to have a peaceful life. In hospital it’s noisy, there’s little privacy, there’s little peace.
During this exchange, the daughter on the link has her (electronic) hand up and she’s been writing in the chat (“He will not – they don’t even know he will survive”). I’m not sure whether or not the judge sees it. It’s swiftly deleted – not, I think, by her.
Mr Justice Hayden then turns to counsel for the Trust.
Judge: Taking that 80% chance as opposed to staying in hospital on a ventilator doesn’t on my reading of the papers look delicately balanced.
Trust: No.
Judge: I can see, I can feel, the grief of the family. Sometimes grief ambushes logic. It may be necessary to give the family a little more time.
Trust: The ventilator treatment is burdensome and would have stopped weeks ago. It’s only because of this dispute that he is still on the ventilator.
Judge: (to son) This is about what is right for your dad. And that is different from what you want for your dad. You want him there for ever and ever, and that’s not going to happen. For any of us.
Another message comes through on the chat from the daughter on the remote link: “There is going to be 0% he’s going to survive”.
The hearing has been going for half an hour. At 12.10, the judge asks observers and lawyers to leave the video platform “to give family time to talk among themselves”. I leave – not optimistic that this strategy will result in any positive developments.
Position Statements
Now that I have a stronger sense of the dynamics of this case, I read through the Position Statements properly.
The applicant Trust
The Trust seeks a declaration that P lacks capacity to conduct proceedings and to make decisions about his medical treatment (that at least is uncontentious). They want an order that it’s in his best interests to undergo withdrawal of mechanical ventilation and a determination as to whether it is in his best interests to receive only palliative care.
They’ve submitted a joint witness statement from two Consultants in Intensive Care medicine and anaesthesia. It describes how P collapsed at home, was found on the bathroom floor, and was transferred to hospital with a suspected stroke. In hospital, his condition deteriorated further, with a fall in consciousness level to a Glasgow Coma Scale of 9 and several seizures. A crash call was made, he was sedated, his trachea was intubated and he was admitted to ICU where he’s remained ever since. He is unconscious, and “does not display any signs of awareness to stimuli”. He has never shown any evidence of being aware of or recognising his family. Although he sometimes opens his eyes, this seems to be random, and not in response to stimuli (such as his name being called) – and there’s no evidence of any emotional responses.
In the event that withdrawal of ventilation fails, the Trust is not willing to perform a tracheostomy or to reintubate P and recommence mechanical ventilation. The clinicians say that “any improvement in his condition is exceptionally unlikely” and they are “concerned about artificially prolonging [P’s] life with mechanical ventilation and burdensome and undignified care and interventions on a daily basis, which is not felt to be in his best interests”.
The patient’s life expectancy in his current situation (on the ventilator) is “likely to be measured in weeks to months”. If extubation is successful, his life expectancy would likely be exactly the same (“weeks to months”). If extubation fails and he is given only palliative care, the doctors estimate life expectancy as “hours to days”. If, however, extubation were to fail and a tracheostomy were to be inserted (obviously not by this Trust as they say they’re not willing to do it), then his life expectancy would be “months, possibly years”[5].
The Trust clarifies that the daughter (the one on line in the hearing, who’s been sending messages in the chat box) “opposes the application” and that she “wishes to speak on behalf of the family, and it is not anticipated that the other family members will actively participate in the proceedings”. Clearly the Trust had not reckoned on this judge’s determination to ensure family participation across the board: in fact, in turns out that the son, the wife, and another daughter all address the court.
The Official Solicitor
The Official Solicitor (OS) gives a more detailed and technical medical account (and there are some minor discrepancies between the OS and the Trust e.g. as to whether the Glasgow Coma Scale dropped to 8 or 9) – but the medical picture is much the same. Quoting the medics, the OS says that an EEG shows “diffuse severe encephalopathy” and “outcomes are likely to be extremely poor if he survives, with significant disability, and risk of a vegetative state”. He doesn’t show any signs of pain or distress. A consultant in stroke medicine says that neither ongoing intubation nor tracheostomy is in P’s best interests “as there is no scope now for neurological recovery”. There is no mention of whether or not another medical treatment the patient is currently receiving (clinically assisted nutrition and hydration via nasogastric tube) is in the patient’s best interests. (This isn’t part of the Trust’s application.)
The OS also quotes the views of family members that P should not be removed from the ventilator. The spokesperson daughter said: “if it is time for him to go, he should go naturally” and “the family will not assist him in his death”. She said he would want to go on living because he has children and grandchildren and that the family has faith (they are Methodists). Given the risks the family has been told are associated with tracheostomy, they were not sure, she said, that a tracheostomy was in his best interests. The hospital Trust has given names of solicitors’ firms to the spokesperson daughter and the lawyers plan to seek (free) representation for her for the final hearing. (This makes apparent to me, for the first time, that this is not intended to be a final hearing.)
There’s also a legal point to consider. Would the clinicians actually continue to keep P on the ICU and continue mechanical ventilation (which they consider “burdensome“, “undignified” and probably clinically unnecessary to keep him alive) in the unlikely event that the judge were to decide it was in his best interests to continue to receive it? And what would happen if extubation were not successful? If re-intubation and a tracheostomy are not now available options (because the Trust is not willing to offer them), then really there isn’t a best interests decision between treatment options available to the court to make. “It may be”, says the Official Solicitor, that the applicant is seeking something closer to a declaration of lawfulness in relation to extubation”.
The hearing resumes: Official Solicitor seeks adjournment
When the hearing resumed about half an hour later, the judge stated firmly that “the chat facility has been disconnected. Nobody is to use it”. I understand why, under the circumstances – but this is mildly concerning to observers since it’s common practice for us (often invited to do so by the judge) to use the chat to highlight technical problems when we can’t hear or see what is going on. I hope this won’t be necessary.
Counsel for the Trust says that the outcome of the family discussion has been to confirm that the spokesperson daughter (“in particular”) opposes the application. She “disagrees with the way the case has been presented and with the medical view on extubation”. Where to go from here? “My Lord, we are entirely in your hands” (that’s what lawyers regularly say when they mean “it’s up to you what to do next, and I’m not going to make any [more] arguments about that”).
“You know my view that in these circumstances delay is harmful to P”, says the judge. And indeed those of us who’ve watched similar hearings before this judge do know that – and we’ve reported on it before (“Delay is inimical to P’s welfare”). The judge adds (though it’s “not a criticism”) that “this case has arguably taken too long to get to court”. The implication is clear that the judge wants to make a decision about P’s medical treatment very soon – today, or tomorrow. So, it’s looking as though this would be a final hearing.
Counsel for the OS says he wants to “express opposition to that course of action”. The judge seems surprised: “that is not a submission I would expect to hear from the Official Solicitor”: I take it that this reflects the judge’s view that delay is inimical to P’s welfare, a view he expects the OS to share. The OS explains that it’s important to get legal representation for the spokesperson daughter so that the judge can hear the views “on behalf of the family”. The judge gives that short shrift: “She can’t speak on behalf of the family, can she. They have different views. It’s rather a challenge to speak on behalf of those with whom you disagree”. Counsel for the OS stands his ground: “She’s a party who wishes to take part in proceedings and has some concerns about how long she’s had to get legal representation” – but when pushed to say “how long?” she’s had, he’s forced to say “I don’t know”. He adds that the other family members “are not parties and because they are not parties they’ve not had sight of the bundle, including the medical records”. I gather from what he says (although the judge cuts across him so it’s not wholly clear at this point) that the predicted 80% success rate for extubation is news to the family. The judge says pointedly that these are “powerful submissions” on behalf of the spokesperson daughter, “but what about YOUR client, Mr Lawson? … The court’s focus is on a man with an 80% chance of coming off a ventilator, who has been on it far too long, and the parties are proposing maintaining it another two-and-a-half weeks” (I take it that’s the proposed date of the final hearing – though I haven’t seen the draft order).
By now the judge sounds exasperated. “It’s as plain as a pikestaff””. He says “I have no difficulty understanding their case, even if the Official Solicitor does”. He adds that “speaking to P’s son, it struck me that he had a very good understanding of the situation, while wrestling with his own grief and his love for his dad”. (That wasn’t quite so apparent to me, as an observer.)
Counsel for the Trust has predicted the judicial impetus to hear the case today and she’s on the ball: she says that “in anticipation of you wanting to hear this case now”, she has ascertained the availability of the clinicians and yes, they can give evidence.
The judge turns to the spokesperson daughter and says, “I’m going to let you be joined as an intervenor. I’m not going to accept you as the voice of the family”. I doubt she knows what an “intervenor” is – when she asks for an explanation of what he’s said, he replies only “because they have different views from you and I’m going to hear from anyone who wants to speak to me”. He asks her about legal representation and she says she “got notice about a week and a couple of days ago” and “nobody wants to take the case”. Counsel for the Trust says, “just for clarity, a list of solicitors was sent on 1st July” (that’s more than three weeks ago) – and the judge turns to counsel for the Official Solicitor.
Judge: Mr Lawson. Twenty-one days!
OS: Our concern, obviously, is only to ensure that the family are able to take part collectively and individually, in a way that is productive for them. We always recognise, of course, in these cases, the burden on the person who is receiving treatment.
Judge: The focus here is that he has a limited reliance on ventilation and there’s a real prospect of success in coming off it – and already the best part of a month’s delay. It’s difficult to see how P’s interests are the focus. Rather than drifted off to the margins.
We break at 13.05 for lunch, resuming, we’re told, at 2pm (actually 2.08) by which time it is hoped that there will be some representation for the daughter, the erstwhile “family spokesperson” and would-be party, now “intervenor”.
But when we resume, nobody has been found to act for her.
There’s a discussion between the judge and counsel for the Trust about the basis for the application. When “there are no options” (since the judge cannot compel the Trust to give treatment they consider unethical), is the hearing “actually needed at all?”. In explaining why the application was brought, counsel for the Trust refers to another case heard previously by Hayden J, GUP v EUP & Anor [2024] EWCOP 3, at which he had expressed the view that “where there is conflict, it is in everyone’s best interests, but most importantly P’s, to bring an application to court”. That, too, was a case where the Trust reached the view that a certain treatment was no longer clinically appropriate, and told the family that it was not available to P, and the family disagreed.
Trust: It would have felt inherently difficult, and wrong, had the Trust engaged this family as extensively as they have in best interests matters then only to say, ‘we’re going to take this decision in any event’. But of course, My Lord, if you take a different view…
Judge: No, no. As you put it, Ms Gardner, having involved the family in best interests decision-making to the extent that they have, it would leave a real feeling of unfairness if the Trust went on to take the decision without ventilating the issues before the court. It could be argued either way. Yours is a compassionate approach.
This exchange highlights a position (apparently shared between the counsel for the Trust and the judge) that the hearing is the ethically right, fair, and compassionate thing to do for the family – a sort of therapeutic jurisprudence.
The hearing proceeded, for now, with witness evidence from the son.
P’s son – witness evidence
The son was sworn in and the judge took him through the answers he’d previously given about his dad (his interest in international politics, cooking etc) before turning to the medical evidence.
Judge: You told me you had a real belief – which I took to be a faith – that he will get better.
Son: Yes.
Judge: Do you know that the evidence in this case indicates that your dad is not going to get better. Do you know that?
Son: I hope my dad gets better.
Judge: I know that. That wasn’t the question though. You pray for a miracle, do you?
Son: Yes.
Judge: Ms Gardner is going to put some medical options to you.
Trust: The consensus of the doctors is that it’s time to have the ventilator withdrawn.
Son: They discussed that with me, and I disagree.
Trust: I know. But you know, don’t you, that all the doctors agree?
Son: That’s why I said they discussed it with me.
Trust: Why do you disagree?
Son: Because I was thinking once they remove, then his life is gone.
Trust: The doctors, Dr [Name] you’ve met, thinks there is an 80% chance if the ventilator is withdrawn that your father will survive.
Son: He said that, but because I am not a medical practitioner I did not (inaudible)
Trust: The force of the concern of the doctors is that it’s a lot to put his body through.
Son: I was just, like I said, having a hope that he’d come back to life.
Judge: When you go to see your dad, what is the thing about his surroundings that strikes you most forcibly? Do you understand?
Son: No.
Judge: When I have been to ICU, what strikes me most is how noisy it is.
Son: I don’t know.
Judge: Whirling, beeping, ongoing activity.
Son: Yes, for the second week….
Judge: And how invasive it is, how many tubes.
Son: I think it’s two, or three.
Judge: Would you consider your dad to be a brave man?
Son: Yes.
Judge: What makes you say that?
Son: That’s how I know him for a long time. Whatever he will do, he’ll have hope in it.
Judge: Your views here are only relevant insofar as they help me to understand what your dad would want for himself. You are here to help me to understand that, not what you want.
Son: I know miracles work.
Judge: Do you think he would want to come off the ventilator and take his chances?
Son: Consult the medical team.
Judge: No! This is not a medical matter. What would he want?
Son: That he recover.
Judge: Stay on ventilator or come off ventilator?
Son: What is good for him. As of now, he cannot talk.
Judge: That’s why you’re here, to tell me what he would want. As his son.
Son: I know he’s definitely going to get better.
Judge: You know that isn’t answering the question, don’t you. Why won’t you answer my question about what your dad would want?
Son: I need to consult the medical team.
Judge: No you don’t. If he comes off the ventilator he has an 80% chance. […] I think you do know what he would want.
Procedural fairness – judge declines the OS request for adjournment
The position of the Official Solicitor had been that the hearing should be adjourned so that the family could get legal representation.
After witness evidence from the son, the judge turned to counsel for the Official Solicitor and asked, “any change in the OS position?”. Counsel referred to “the Re A case in the Court of Appeal” which I had to google afterwards. I’m pretty confident it’s this one, originating in the Family Court: Re A [2022] EWCA Civ 1221.
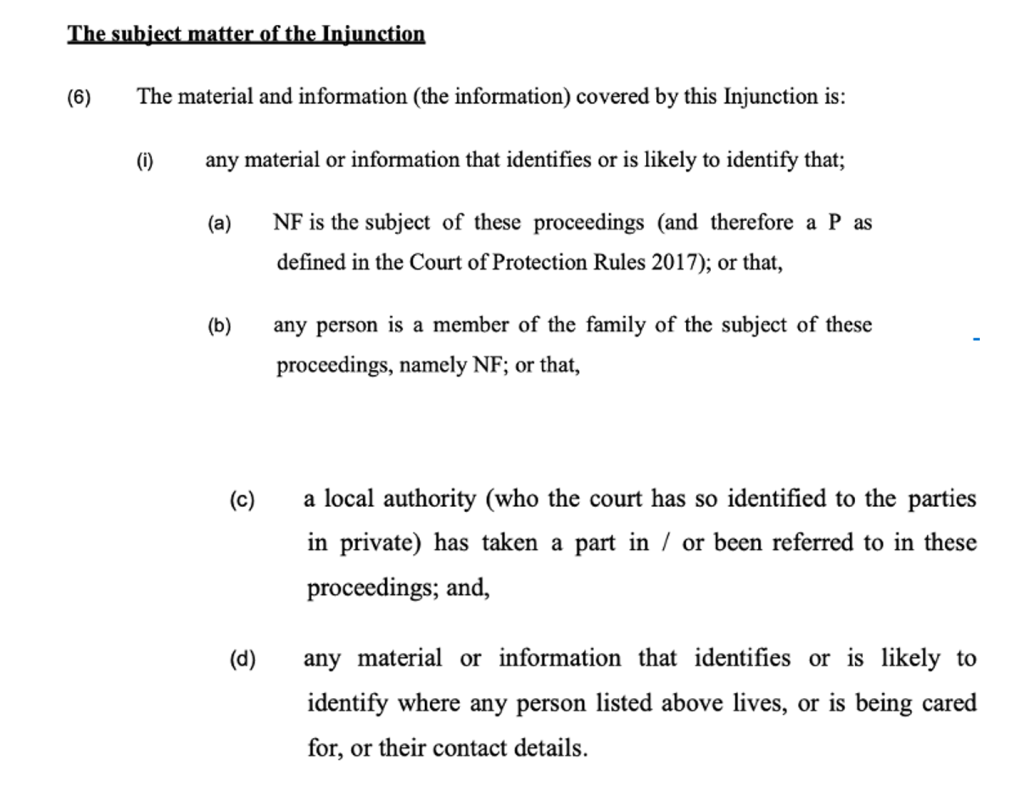
In Re A, a hospital Trust applied to withdraw a ventilator froma baby with devastating brain injuries. The parents lost their legal representation three days before the hearing (their application for legal aid was turned down) and asked for an adjournment of three weeks to find lawyers to act for them (either pro bono or with crowd funding). Hayden J refused their application, went ahead with hearing the case (including evidence from the parents, devout Muslims, who believed that the decision should be made by Allah not by man). He handed down a judgment the next day ordering that ventilatory support should be withdrawn due to the severity of the baby’s brain injury which meant that he was unable to benefit from treatment, and the burden of treatment itself.
The Court of Appeal found that Hayden J’s decision in Re A not to permit an adjournment so that the parents had a chance to get legal representation was procedurally unfair. They identified two reasons why procedural fairness is important: (1) because it helps to improve the chances of reaching the right result (“the path of the law is strewn with examples of open and shut cases which, somehow, were not”) and (2) because “justice is intuitively understood to require a procedure which pays due respect to persons whose rights are significantly affected by decisions taken in the exercise of administrative or judicial functions”.[6] The judge should, the court said, have properly considered the immense importance of the issue to the parents (the life and death of their child), and the fact that they had lost their representation, through no fault of their own, just days before the hearing. Hayden J should also have recognised the daunting task they now faced in representing themselves as litigants in person – with complex medical evidence at a time when their child was lying critically ill in hospital. They were also non-native English speakers.
Counsel for the Official Solicitor distinguished the case before Hayden J today from Re A to the extent that the parents had expected to have a legal team to represent them, whereas the family in the current case seem to have made no progress with obtaining lawyers over a three-week period. But he emphasised that there is a 20% chance that removal of the ventilator will result in P’s death so this is an immensely important issue for the family. He also said that just a few weeks earlier, it had been said at ‘best interests’ meetings that post-extubation tracheotomy or re-intubation were on offer as ethically available options – that had changed relatively recently – and also that only one member of the family had received the medical evidence in the case. “None of them has the full bundle. They literally haven’t read it yet. […]. We remain concerned that the family have not yet had the application papers and are therefore in a very difficult position. Lawyers would find it a challenge to take on this case and prepare for a hearing tomorrow, but a non-specialist…..”.
The judge asked: “Has the Official Solicitor herself taken this decision?” – referring to Sarah Castle – and when it seemed she had not, he said, “I’ll rise. I want to hear it from her.”
After a short interval, counsel for the Official Solicitor reported back. The Official Solicitor, he said, asks for an adjournment, for one week – less to allow an opportunity to obtain representation and more because she is “keen for all voices in their family to be heard on an equal footing”, which isn’t possible at the moment because only the one daughter has received the medical evidence in the case. She wants to enable all family members to “have the papers and the opportunity to understand the evidence before the hearing”. The judge pointed out that there would be medical evidence given in court the next day. “But without any notice – they’ll hear it live, as lay people, about a critically ill relative” said counsel. It was, he said, “difficult to see that they can contribute, if they wish to, from a cold start tomorrow morning”.
This position was not well received. The judge said “I can’t imagine this court would do anything other than listen to all the family members, and ‘on an equal footing’ is so trite as not to need saying”. Counsel for the Trust said their concern was “if you accede to that request, we may be in exactly the same position in another week”. Moreover: “there doesn’t seem to be any active request from any of the family members to have the court papers” – nor was there any request from them to become parties.
Here’s what the judge said (as best I could capture it) in making his decision to proceed with the hearing, refusing the application for an adjournment so that the family could get legal representation.
A little while ago, in response to the question ‘what would your father want if he could speak?’, the son was unable – pointedly unable – to answer the question. The only reasonable inference to be drawn from that is that he knows his father would very much want to take the opportunity to leave ICU. Most of us would. In that indirect way, P’s voice comes into the courtroom. Short of the miracle his family pray for, there is little prospect of any medical recovery, but there is the opportunity to greatly improve the quality of his life at the end. ICU is the last place any person would want to be. Given the delay that’s already taken place in effectively depriving this man of that opportunity for greater comfort, I cannot see anything eclipsing the need to do that now. The medical issue, properly analysed, is not a complex one, and it’s one I would have thought well within their grasp of understanding: the opportunity of a more comfortable life off the machines, even though there is a 20% risk that will cause his death. It’s a probability of something positive for him. On an intellectual level, there is no coherent contrary argument – though of course it’s different on an emotional level. This is the only significant thing that can be done for this man, and it’s a very significant thing. So, I decline the Official Solicitor’s request to adjourn so that all the family can have the papers. I do not think that eclipses the obligation to make a decision in this case. I have said before that the Mental Capacity Act does not import the avoidance of delay in the way that the Children Act does, but that requires to be read into it as a facet of P’s Article 8 and Article 6 rights.
And with that, he asked the wife if she would now like to give evidence.
Wife’s evidence
The wife’s witness evidence is interpreted by the son who comes into the witness box with her.
Judge: It is very brave of you to give evidence. What I want you to tell me please is a little bit about P. What kind of a man is P?
Wife: Oh, very brave.
Judge: Was he a good father?
Wife: Yes.
Judge: If they take him off the ventilator, there is an 80% chance that he would be okay without it. Do you understand?
Wife: Yes.
Judge: It’s understandable that you would worry that he might be in the 20%, but these are good odds. Now what would P tell me if he was here. Would he want to take those odds or not?
Son: (interpreting) She said that whatever decision you make, she will pray that he will recover.
Judge: (something about knowing his wishes – I missed it). He and I are of very similar age. I get the impression that he would go for the 80% chance?
Wife: Yes.
Judge: Yes? If you think ‘yes’, that’s the end of it. That’s good enough for me. You say ‘yes’?
Wife: Yes.
Judge: Thank you.
After a brief exchange about where P would be discharged to if he were to survive extubation (the family live in a different city from the hospital where P is being treated) –Hayden J says: “Both of these last two witnesses have given utterly compelling evidence, not just in what they said but in the way they said it. They smiled, with absolute confidence that they know what this man would have wanted – and they are both very close to him”. (I didn’t find the evidence as compelling as the judge did – the first witness had declined to answer the question about what P wanted, and the wife simply responded “yes” (twice) to a leading question.) Counsel for the Trust points out that these two witnesses (unlike the daughter, who says in court that she has mobility issues, which is why she’s attending the hearing remotely) “have seen him, they’ve visited, they’ve been at his bedside”. “More than that,” says the judge, “they know his temperament. And the combination of that and the medical evidence, well, it makes my difficult job as a judge about as easy as it gets”.
The judge calls on the daughter. Does she want to come back tomorrow? She does. He ends the hearing by saying, “Well, we have worked our way substantially to a resolution. Tomorrow morning then at 10.30am”.
In fact, the start of the hearing on 23rd July is substantially delayed – until nearly noon. It turns out that the son had been unwell during the night, and was discharged from hospital at 3am, causing concern for the family and delaying their attendance at court.
Medical evidence
The lead consultant (attending remotely) gave evidence, having examined P that morning, that his condition is unchanged. He has a Glasgow Coma Score of 8 and no evidence of awareness. He is receiving 21% oxygen (“essentially air”) and there is “a greater than 80% chance” that if mechanical ventilation were removed, he would not need it and would breathe on his own. The daughter is offered the opportunity to ask questions – I didn’t manage to get down everything that she said (and the replies) but here’s my best attempt.
Daughter: I need some explanation, because I do not understand how you managed to calculate that he had a 20% chance of surviving and then to find out through court documents that he had 80% chance. That is a big jump. You are telling me that he’s brain dead even though some parts of his brain are working. My fear was that once he comes off, you guys cannot guarantee as a doctor that he can survive the 10 minutes or 20 minutes it takes to pop him over.
Doctor: We discussed the chances of success at the best interests meeting, but I don’t recall giving a 20% figure at that time. I have checked the records and there is nothing quoting that figure. We did discuss the chances of success or not success and being honest with the family, we did need to say we couldn’t give certainty.
Daughter: I believe that’s misleading us, the family, and now it’s in a document that’s been presented to the judge, and you should have shown it to us.
Doctor: We’ve had six weeks that’s passed since that best interests meeting and during that time we have (missed what was said)
Daughter: You cannot guarantee that he is going to survive when you take him off there. If there’s an 80% chance and he does not survive, how are you going to explain that to us, the family?
Doctor: We will discuss palliative care and how to manage his death in a comfortable and dignified manner.
Daughter: But he will be dead. So he won’t be able to receive that care you put forward for him.
Doctor: He wouldn’t immediately die, and so we would have time to address those end-of-life care needs.
Daughter: But what if he’s gone past the point that you can deliver that care?
Doctor: I would like to reassure you that we deal with these situations, day in and day out.
At this point the judge intervenes. He asks whether the daughter, who has mobility problems, has been able to see P on ICU via a video-link. She hasn’t. He asks the doctor to describe what it’s like for P. The doctor runs through a list of interventions P receives: a pressure alleviating mattress, turning every two hours to prevent pressure sores, a urinary catheter, management of bowel incontinence, compression devices on his legs, medications injected into his stomach each day to prevent blood clots, and suctioning. He has “sympathetic activity” (i.e. activity in the sympathetic nervous system) when he’s turned or suctioned – “rapid heart rate, sweating, contracture movements, all of which look deeply unpleasant”. He says, “it’s distressing to see him on a daily basis in the condition that he’s in”.
The daughter asks if she can say something – the judge tells her “later”, and asks his own question: would P be exposed to a risk of ICU syndrome (probably not due to his lack of awareness). Then he asks “what would be life for P if he comes out the other side?”. The doctor explains that he’d still be dependent on nasogastric feeding and suctioning to help clear secretions, daily bed bathing, barrier cream, and the urinary catheter will stay. The daughter turns away from the camera and puts her head in her hands. Later she turns back and is wiping her eyes. When eventually invited by the judge to speak, she looks upset and says she has now forgotten the question she was going to ask.
Counsel for the Official Solicitor asks the doctor some questions in cross-examination: how often does he see the patient (a minimum of once a week); was there a conversation with the family about terminal extubation on 29th May, and what were the chances of success then? “What is the use of this?” asks the judge, “hypothetically deriving a percentage risk retrospectively”. The doctor says: “I would have described a position where I thought there was a reasonable chance of extubation being successful, trying to communicate there’s a reasonable chance this will work, and therefore this is something we need to try, but making sure they understand there’s a chance of failure, so they’re not surprised if it doesn’t work”. The judge intervenes: “You may not be aware that now they understand the high probability of success, both [P’s wife] and [P’s son] say that undoubtedly [P] would want to take that risk himself. That really is the end of the case as far as I’m concerned, but we’re just (pause) dotting the I’s and crossing the t’s.”
Counsel for the Official Solicitor has another go at asking a question, but he doesn’t get to finish it. “Do you have an understanding how it is that some members of the family-“. “Mr Lawson, this is NOT helpful”, says the judge. (I suppose the question was headed towards interrogating the 20% success figure that the daughter had previously taken to be correct.)
Asked about the options available to P if extubation were unsuccessful, the doctor is clear that “as you can see from the best interests discussions, tracheostomy is not a treatment that myself or [another intensivist] felt should be offered at that point”. He says it “is not a treatment that would improve P’s neurological situation. It could lead to significant harm, including an uncontrolled death. There’s no benefit, and it could lead to harm, so it is not a treatment we would offer”. The judge asks, “Is it unethical?”. The doctor replies, “Absolutely”.
Counsel for the Official Solicitor pursues the point.
OS: It was on offer earlier, wasn’t it – but not considered to be in his best interests. Is that wrong? Was it not available as an option?
Doctor: When we are explaining treatment options to the family it would be disingenuous not to discuss tracheostomy as a possible treatment, because that’s something they’ll be aware of from the wider community.
OS: Is it right that it wasn’t said to be unavailable.
Doctor: That’s right. We did not say explicitly to the family that it was not available at that time.
OS: You discussed the practicalities of performing a tracheostomy.
Doctor: Time has passed. Tracheostomy won’t lead to neurological recovery. The reason not to do a tracheostomy is because his neurological condition is so severe and so persistent and unchanging and the tracheostomy would not treat it.
OS: Doesn’t a PEG also not support neurological recovery and just maintain the person. It’s intrinsic in one of the options, isn’t it, to discharge to a nursing home.
Doctor: My understanding is that he has a naso-gastric tube which would negate the need for a PEG.
OS: Isn’t it logical that either a tracheostomy and feeding support should be offered, or neither should be offered.
The judge intervenes to stop this line of questioning. It’s not helpful.
Finally, counsel for the OS asked, “Can you help us with your opinion about what other experts in your field, and other units, would advise about available options?”. The doctor replied: “As an intensive care community, given the severity of his neurological injury, its persistence, and failure to improve, the community would support extubation, and if that extubation were to fail, they would support palliative treatment”.
That was the end of the doctor’s evidence.
Daughter’s evidence
Before the daughter gave evidence, the court was told that the second opinion doctor confirmed everything the doctor who had given evidence had said. Then the judge addressed the daughter. Her response, by the end, was surprising.
Judge: Both [P’s son] and [P’s wife] said P would want to take the 80% chance to get off ICU.[7]
Daughter: We would want him to be alive. It would be nice to help him get back to family life.
Judge: I am taking your evidence to help me understand what he would decide for himself. What do you think?
Daughter: He would take that chance, that opportunity.
Judge: I think that’s the end of the matter. If that’s what he would want, that’s what he’s going to get. When every single member of his family tells me he would go for those chances, I couldn’t possibly make any other decision, could I?
Daughter: You are right, Your Honour.
The daughter adds that her sister is also available on the link and would like to give evidence. She does (briefly, and without being sworn in) but there’s interference on the line and I can’t hear what she says. I gather, from the judge’s response, that she supports her sister.
“I’m regard this decision as one of the easier ones that I have to undertake”, says the judge – announcing that (as it’s now 1pm) he will now adjourn and return (briefly) at 2pm. I’m unable to watch the rest of the hearing, but learn from another observer that it was short.
Reflections
I am left with a sense of disquiet about this case. I don’t really doubt that the outcome (withdrawal of the ventilator, followed by palliative care if that’s unsuccessful) was the right way to go – indeed, on the basis of the evidence presented in court, it’s difficult to see how any other outcome was possible, given that this Trust was not willing to offer ongoing treatment and the lead doctor gave evidence to the effect that it was unlikely that “the intensive care community” in any other hospital would provide ongoing ventilation or a tracheostomy (though see footnote 5).
But precisely because there were no other available options before the court, and the outcome seemed a fait accompli, it is hard to see why the hearing was necessary. The judge suggested that the need for a hearing could be argued “either way”, and I understand his wish for compassionate engagement with the family. But since there was apparently no “best interests” decision to make about treatment options, and only one possible outcome, the hearing seemed redundant – at least insofar as Court of Protection hearings are designed to make decisions between available options.
The decision of Hayden J in the GUP case (GUP v EUP & Anor [2024] EWCOP ) – the case cited by counsel for the Trust as a reason for bringing the case to court – appears to directly contradict the approach taken by the Court of Appeal in AVS v A NHS Foundation Trust & Anor [2011] EWCA Civ 7 and the Supreme Court in N v A CCG [2017] UKSC 22. Here’s what two very respected lawyers have to say on the matter:
“.. we remain very doubtful that the Court of Protection is the correct forum for seeking a declaration of lawfulness in respect of a determination that a course of treatment is not clinically appropriate – rather, we suggest that the correct forum is the King’s Bench Division under Part 8 of the CPR, not least so as to avoid the slide into best interests language / analysis that (on one view) took place in Re EUP. We also have squarely in mind the Court of Appeal decision in AVS v A NHS Foundation Trust & Anor [2011] EWCA Civ 7, which made clear that disputes about best interests where the treatment option is not on the table should not be entertained by the Court of Protection” (Alex Ruck Keen KC (Hon) and Tor Butler Cole KC https://www.mentalcapacitylawandpolicy.org.uk/dont-ignore-the-serious-medical-treatment-guidance-but-lets-be-clear-about-what-the-law-requires/)
By the end of the hearing, it seemed as though there was a consensus as to the way forward – with the daughter who had been the most confrontational of the family members explicitly stating that the judge was “right” to make a decision in favour of the Trust’s application. It seemed that the family had been coaxed (if that’s the right word) into recognising that the only available option was what P would want for himself under the circumstances – and if so, that is surely eases their pain in accepting it, though I found the process whereby they were led to this position at times uncomfortable to watch. Reconciling the family to an inevitable outcome must be a good thing and I think that’s what happened, and I have no evidence that they thought anything unfair had taken place in court. I suppose I would have hoped that this could have happened out of court (especially as their opposition seemed based on not having been told – or not understanding – the likely success of extubation: could better communication or mediation have averted the need for a judge to bring about this reconciliation?
The Trust’s decision to make an application for withdrawal of one life-sustaining medical treatment (the ventilator) but not another (the feeding tube) was raised by counsel for the Official Solicitor in his cross-questioning of the doctor, but was cut off by the judge. I would have been interested to hear the Trust response. I presume their decision was entirely pragmatic. As long as P is on a ventilator, he’s stuck in the ICU – which is probably not necessary to sustain his life, is not good for him, and uses a valuable resource that could be made available to someone else with a better chance of recovery. Without the ventilator, P can be moved out to a different part of the hospital and then (if he survives) to a nursing home, and the question of clinically assisted nutrition and hydration can be negotiated (or, more likely, ignored) by someone else. I didn’t see any indication that the family would be likely to agree that withdrawing tube feeding would be in P’s best interests – and raising it now would only add to their distress. If the doctors are right about P’s prognosis, and if he survives extubation but continues to receive tube feeding, he will most likely become another of the many patients being maintained in prolonged disorders of consciousness around the country – possibly, if he breathes on his own better than they expect, surviving for years.
It seems unlikely that the outcome of this case would have been any different if the family had been given the opportunity to instruct a lawyer to argue their case. It felt to me like a forgone conclusion. But at least legal representation would give everyone more confidence in the outcome and it would clearly have been more in line with the requirements of procedural fairness. – though the family members themselves did not seem unduly concerned about this. But at the same time as I want to advocate for P’s family to have legal representation (if they want it), I worry about the price that P might pay in terms of the delay that this imposes – something that was also clearly at the forefront of the judge’s mind in this hearing.
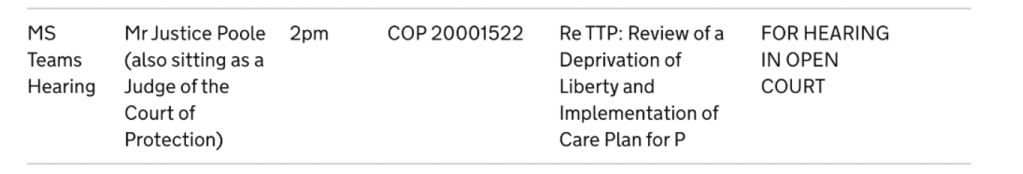
The disquiet I feel about this case is matched by the disquiet I feel about another case concerning a patient in a prolonged disorder of consciousness heard recently by a different judge, Mr Justice Poole[8]. The facts of that case are very different. The patient had made an Advance Decision to Refuse Treatment (ADRT) which – if valid, applicable, and authentic (all of which the biological family contested) – was a binding refusal of life-sustaining treatment in the very situation he was now in: eventually, the judge ruled that the ADRT was binding, treatment was withdrawn and P died. But it is indisputable that for six months, between January and June 2025, while the court was hearing this case, P received treatment that he had wanted to refuse, and in fact had refused in a binding legal document. Withdrawing the unwanted treatment was delayed by the necessity of court proceedings – and in addition was delayed longer than was justifiable (in my view) by the judge’s scrupulous attention to procedural fairness, with the family given every opportunity to advance their position and pursue arguments which (as far as I know, given that the family refused me access to their position statements) were wholly speculative and lacking in any evidential basis. Procedural fairness may, arguably, in this case, have caused harm to P, by extending the period of time that he was treated against his will.
What concerns me, in both these cases, is the tension between P’s welfare (he shouldn’t be given burdensome treatment, or treatment he’s refused) and the perceived need for a hearing, and for a procedurally fair hearing – which takes time to arrange and is delayed by waiting for parties to find representation, and ensuring that family concerns or accusations are addressed. I acknowledge, of course that P, too, has an interest in the procedural fairness of a hearing, insofar as it is the approach most likely to result in the correct outcome.
I know that judges are aware that P’s welfare and procedural fairness in hearings can sometimes pull in different directions: both Hayden J and Poole J indicated as much in the course of their respective hearings. They resolved it in different ways – perhaps (from my perspective) too quickly in one and too slowly in the other. I suspect there is no one “right” way to resolve this fundamental dilemma.
Celia Kitzinger is co-director of the Open Justice Court of Protection Project. She has observed more than 600 hearings since May 2020 and written more than 100 blog posts. She is on LinkedIn (here), and also on X (@KitzingerCelia) and Bluesky @kitzingercelia.bsky.social)
Footnotes
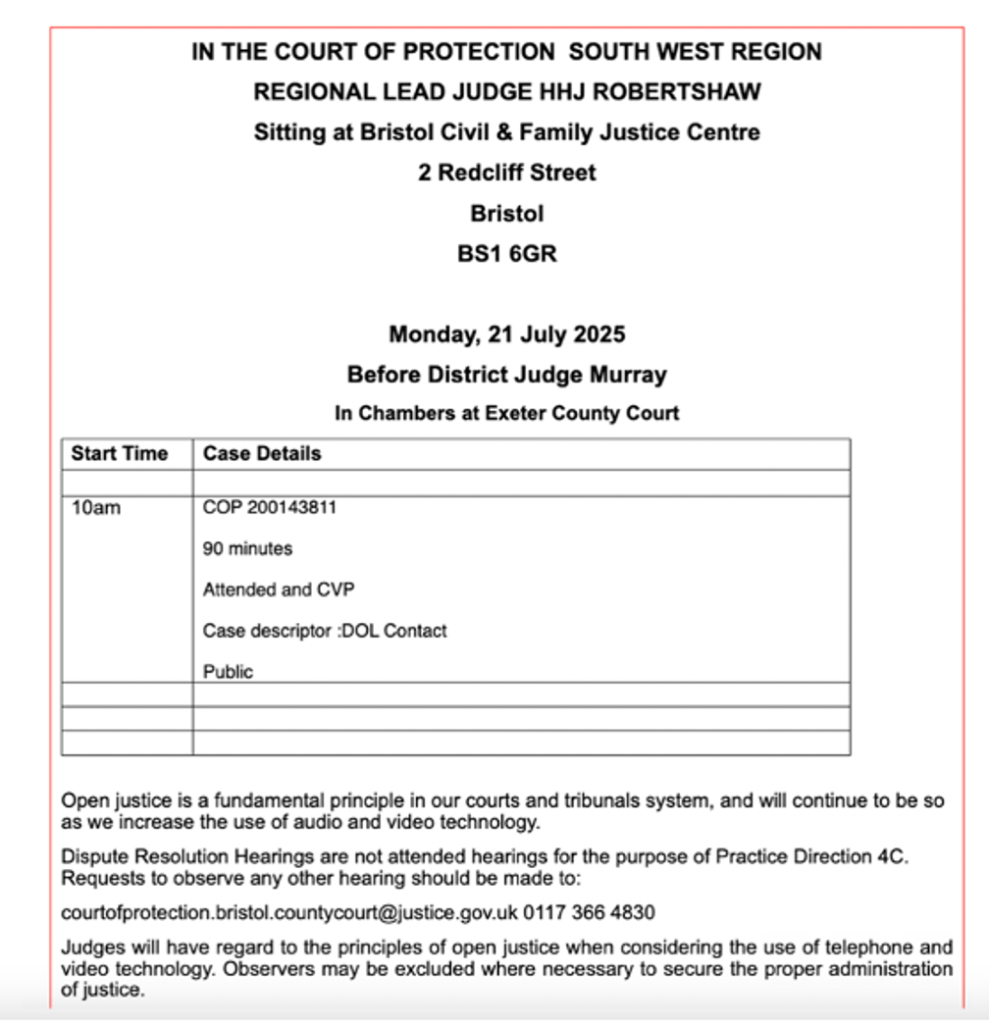
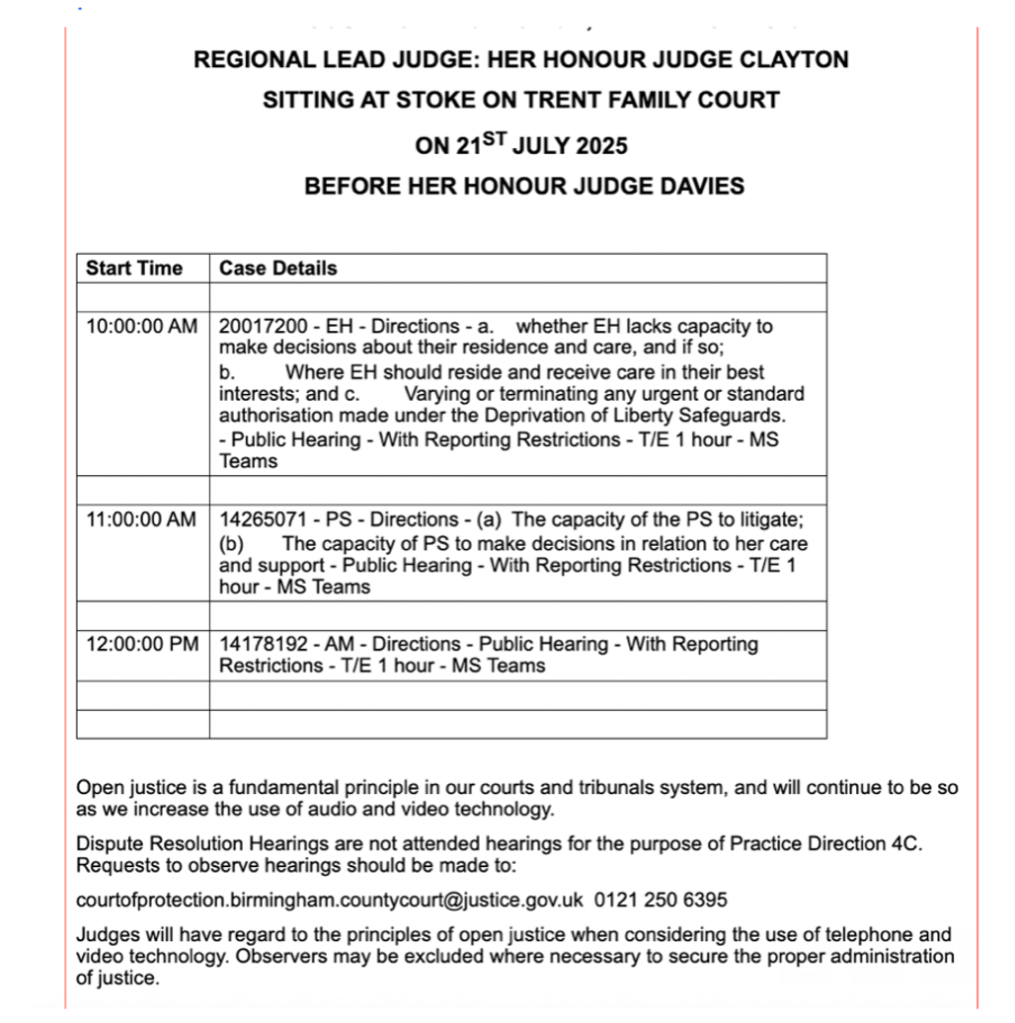
[1] Over the five years that the Open Justice Court of Protection Project has been in existence, there has never before been any indication in the listing as to what hearings in the Royal Courts of Justice are about – with the sole exception of committal hearings. We welcome this development.
[2] My understanding of this hearing was significantly helped by the fact that, in line with the new guidance from Poole J, both counsel sent me (anonymised) Position Statements before the hearing started. Thank you!
[3] E.g. Re GU [2021] EWCOP 59 and recently in the Family Court, Guys and St Thomas’ NHS Trust v J (a Minor) & Ors [2025] EWHC 1988 (Fam)
[4] According to the position statements, this “daughter” is either an adopted daughter or “not [P’s] biological daughter but identifies as his daughter”.
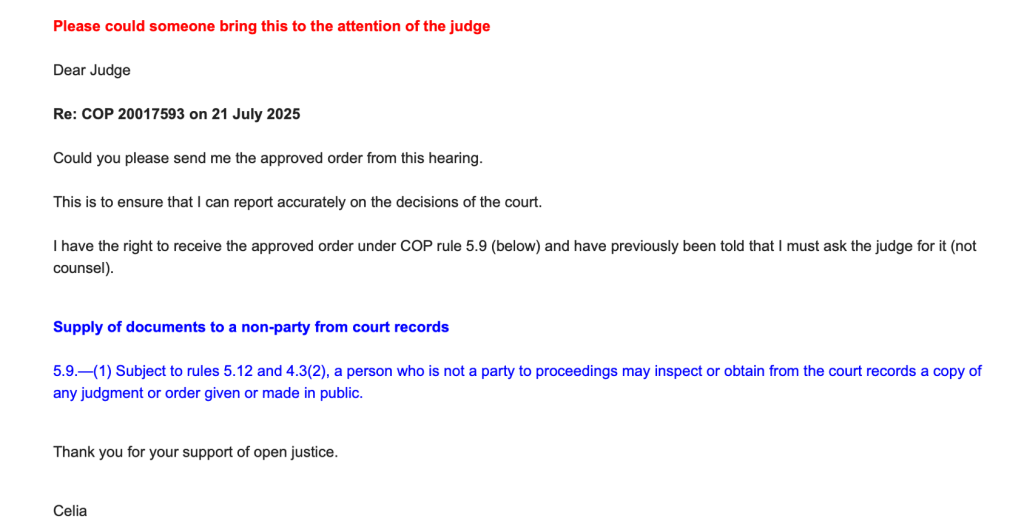
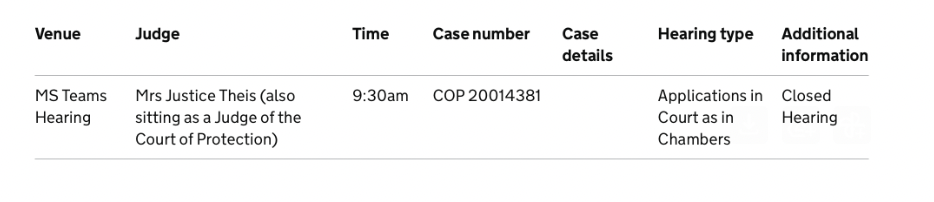
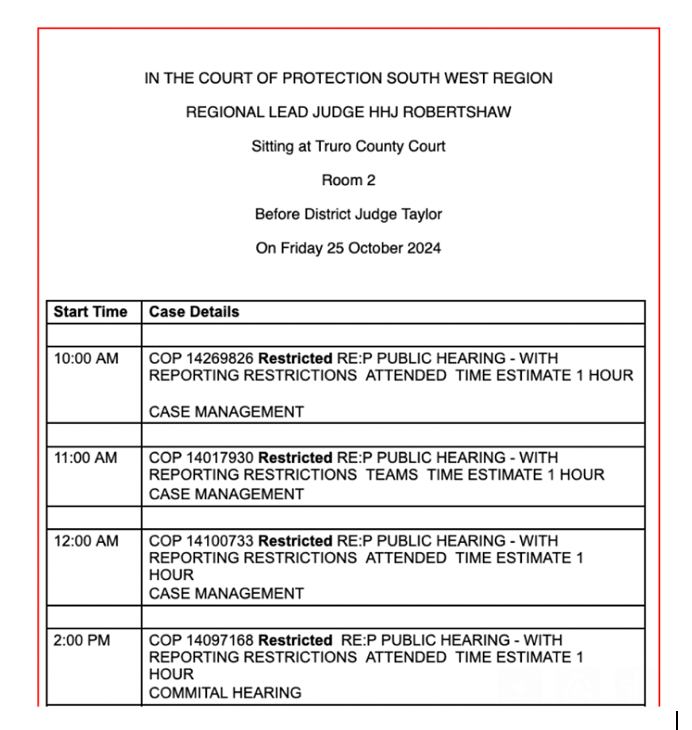
[5] Over the course of my research with the Coma and Disorders of Consciousness Research Centre, I’ve seen vegetative patient who’ve had tracheostomies for many months or even years in specialist units and nursing homes. A few days after this hearing, I watched a case before Theis J and learnt that the protected party, who is in a vegetative state, used a tracheostomy for more than five months before being successfully deintubated in March 2025. The Trust has now made an application for withdrawal of CANH. (COP 20017687).
[6] “the path of the law…” quoting Megarry J in John v Rees 1970] Ch 345, at 402; “justice is intuitively understood…”, quoting Lord Reed at §68 in Osborn
[7] Actually they didn’t. The son refused to answer the question – on the basis of which the judge inferred that this was the son’s view of what his father would want. I expect the inference is correct, but the inaccuracy jars. The wife simply gave confirmatory responses to a leading question posed by the judge.
[8] See my two blog posts “Determining the legal status of a ‘living will’” and “Validity and applicability of an advance decision to refuse treatment” – and the judgment by Poole J: Re AB (ADRT: Validity and Applicability) [2025] EWCOP 20 (T3)