By Celia Kitzinger – 28th September 2020
It’s 4.30pm on Wednesday 26 August 2020 and I’m watching a young man (let’s call him Paul) with end-stage kidney failure speak in (virtual) court (Case no: 13634663) about his strong wish to stay alive – not least because of his love for his seven year old son: “he’s my whole entire world. He’s the reason why I get up in the morning. He’s the reason why I am still breathing”. At this moment, giving evidence to his legal representative, David Lock QC (appointed via the Official Solicitor[2]), Paul is very clear that he wants to continue to receive haemodialysis because he wants a chance to live. He also wants to be placed on the list for a kidney transplant.
The problem for the Hospital Trust is that Paul often refuses haemodialysis – a treatment that he needs three times a week (taking 4 or 5 hours each time) to maintain his kidney function. Without it, he will die. He’s had 13 admissions to critical care due to his refusal to accept dialysis. When he’s refused, doctors have resorted to force. Counsel for the hospital trust (John McKendrick QC) says that “the levels of force involved have placed highly experienced clinicians at the boundaries of what they consider to be acceptable practice.” When efforts at persuasion fail, Paul is forcibly held down, sedated, intubated, and given a general anaesthetic so that he can be provided with dialysis.
Paul has been diagnosed as having an “emotionally unstable personality disorder” (also known as a “borderline” personality disorder) at the severe end of the spectrum. In his case, this is characterised by suicidal ideation and auditory hallucinations. He also has what the judge characterised as “an alarming, disturbing and very sad history of self-harming”. The diagnosis qualifies as ”an impairment of, or a disturbance in, the functioning of the mind or brain” under s. 2(1) of the Mental Capacity Act 2005 and causes fluctuations in his capacity to consent to, or to refuse, dialysis. According to his legal representative, “the ‘Well-Paul’ wants to live and is cooperative with his doctors” but when he is in mental health crisis, “the ‘Ill-Paul’ refuses treatment and says to the treating team that he wishes to disappear”.
“The position of the Official Solicitor, informed by Paul himself, expressing his views when he has capacity, is that the person Paul becomes when in mental health crisis is one he doesn’t have control over. He doesn’t want the decisions he makes when he lacks capacity to be respected. He doesn’t want to die.” (Counsel for Paul)
A doctor gave evidence about what she’d experienced in providing treatment for Paul some months earlier:
“It needed four people to restrain him. I explained to him that he didn’t have capacity to make the decision to refuse dialysis so we were going to give it in his best interests and we would sedate him to do that. He curled up in a ball in the top corner of the bed and pulled the sheet over his head. Two psychiatric nurses and two security guards held a limb each so that he couldn’t kick out. I got an injection into his upper arm and a cannular into his hand. He was shouting through most of it, ‘Leave me alone – I want to die.’”
In response to the judge’s (Mr Justice Hayden’s) observation that “it must have been hugely distressing for everyone involved,” the doctor replied simply: “It was awful. Everyone on the ward was very distressed”. The judge asked, “If you hadn’t done that, what would have happened?” “I can’t remember what his potassium levels were,” the doctor said, “but if we hadn’t done that, he would have had a cardiac arrest. Without dialysis, Paul will die.” Not only does Paul refuse dialysis: on some occasions he even deliberately consumes high-potassium foods (bananas and coffee) with the intention of raising his potassium levels to cause death.
The use of force has not been necessary in the past 26 days because Paul has accepted haemodialysis, but doctors were worried that this was about to change. This was an “urgent” hearing – apparently prompted by some of Paul’s recent behaviour: he’d “left hospital, went out on a bus, had a fit, and discussed self-harming again”. The doctors already have judicial endorsement of the use of force: it was decided by Mrs Justice Roberts at a previous hearing on 13 August 2020[3] that forced treatment was in Paul’s best interests. (The judgment seems not to have been published). But the Trust had already made another application to the Court of Protection (due to be heard in just six days time before Mr Justice Mostyn) asking for a declaration that it is not in Paul’s best interests to treat him against his wishes. So, the prospect of having imminently to provide forcible treatment (in accordance with Mrs Justice Roberts’ order) while awaiting endorsement (from Mr Justice Mostyn) of their own current position that forcible treatment is not in Paul’s best interests had led to this “urgent” application.
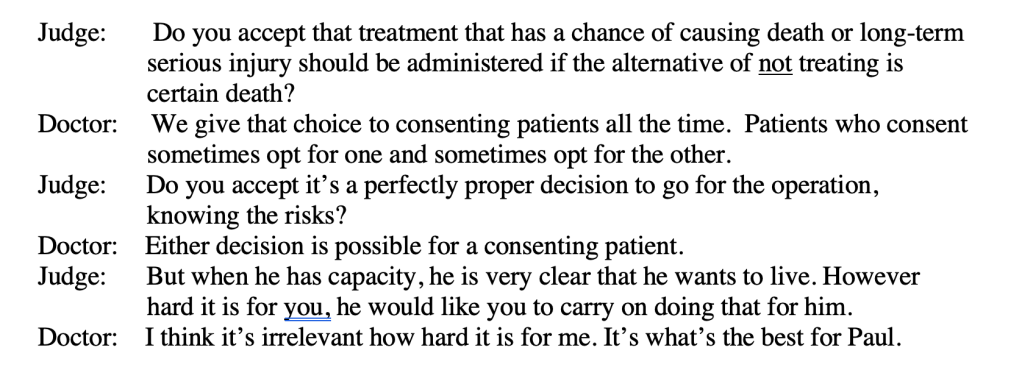
Counsel for the Trust said that the consultant was “hugely concerned” – not least because the risks associated with general anaesthetic include serious brain injury and death: “we feel we cannot continue in this situation” because “what we say is that it is not in Paul’s best interests to continue to receive intubation and anaesthesia to provide dialysis”. Nonetheless, at this hearing the Trust was seeking an interim declaration that it was in Paul’s best interests to treat him forcibly against his (non-capacitous) wishes, pending the forthcoming judgment from Mr Justice Mostyn in six days time, in response to their application that forcible treatment was not in Paul’s best interest.
Mr Justice Hayden began by questioning why this case was in front of him now, since “Mr Justice Mostyn is going to hear this case, not me”. And although the Trust had presented the case as relatively straightforward (essentially, to ‘hold the ring’ and confirm that Mrs Justice Roberts’ order should stand for the next six days), Mr Justice Hayden clearly found it a difficult and demanding situation. He said he was “being expected to endorse the continuation of an order which they [the Trust] say is not only not in his best interests but inimical to his welfare. This is an impossible situation to put a judge in.”
“I cannot think it is proper for me to sanction chemical and physical intervention between now and next Tuesday when the Trust tells me they no longer think it is in Paul’s best interests, and in circumstances where it is so injurious to his health that it might possibly kill him. So, I will have to resolve this if I can today”.
In addition to counsel for Paul and for the hospital Trust (and the treating clinician), other people in court included Paul’s parents, and representatives for the Trust providing psychiatric treatment (Katie Gollop QC), the junior counsel for the Trust (Fiona Paterson), and NHS Blood and Transplant (Peter Mant), though none of these was a party to the case (nor wished to be), and several pointed out that they had not received the bundle.
We heard from the doctor about attempts to persuade and cajole Paul into having treatments when he refuses (they are rarely successful) and about alternatives to general anaesthetic that had been tried with mixed success. There was some discussion of a medication called lokelma which helps to treat high potassium levels but which can’t substitute for dialysis (and which Paul apparently has refused to take). In the end, it appeared that restraint and general anaesthesia was the only way dialysis could be provided. So, was this in Paul’s best interests? It seemed a choice between two bad options.
According to Paul’s father, “the better of the bad options it seems to me is full sedation and treatment along with an integrated approach to Paul’s mental health treatment that will allow him to become compliant with the treatment regimes he needs”. It turned out that Paul’s kidney treatment has been provided in one place and his mental health care provided in another at some geographical distance. Mr Justice Hayden commented that he’d learnt from other cases that healthcare has become segmented into “silos” that “create barriers to treating patients holistically”. Paul’s father wanted “a proper multi-agency plan to address all the different challenges Paul has got”.
When Paul was sworn in to speak on his own behalf he came across as articulate, thoughtful and intelligent. He talked movingly about his relationship with his son and his desire to stay alive. He described cooking with the child, and watching funny animal videos together. When asked about the times when he refuses dialysis, he plainly felt embarrassed and ashamed. “I’m sorry for the drama I cause,” he said. “I don’t mean to. I do feel a little ashamed of how far I let things go. I wish there was a way I could try harder”. If he refuses dialysis in future when he is “overwhelmed” by his mental illness, does he want to be restrained and compelled to have it? He didn’t hesitate to say “yes”.
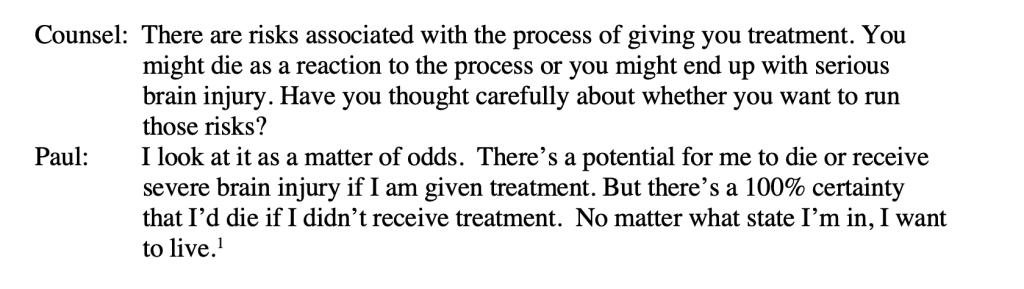
He was pushed on the question of whether he accepted the risk of serious brain damage as a result of sedation, intubation and general anaesthetic.
Having heard Paul’s views, and the arguments of his counsel, the position of the Trust remained that it was not in Paul’s best interests to undergo the high-risk procedures involved in treating him against his (non-capacitous) wishes.
Mr Justice Hayden disagreed. “That Paul wants to go on living, however parlous the circumstances, is pellucidly clear,” he said. In a short oral judgment, he said that the “present regime should be sustained” and he authorised continued physical and chemical restraint in order to enable dialysis, because “without it, death would probably follow within hours or days”.
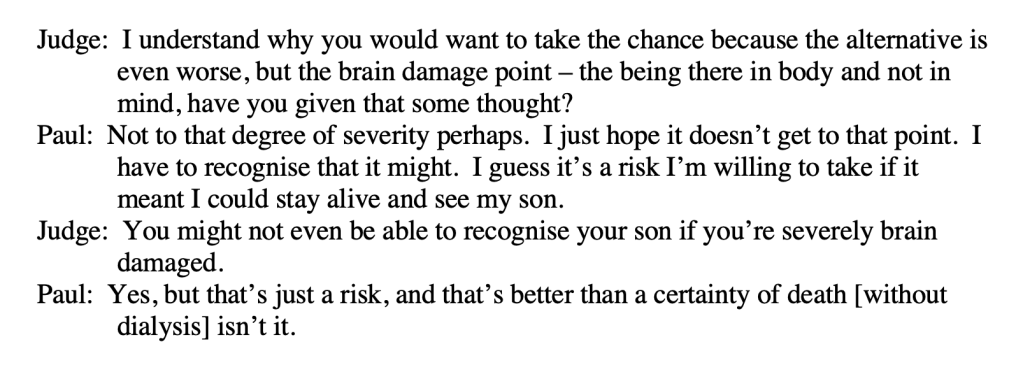
“On the one hand there was death. On the other hand, there was hope, however compromised. For him, and for him as a parent, he would take the hope rather than the certainty of death. For some, the prospect of life with severe neurological damage would be an unattractive prospect, but I was satisfied that Paul was one of those individuals who are willing to take that risk. I cannot think of any circumstances in which I would go against his expressed wishes and feelings delivered with sensitivity, with care, and with intelligence.” (Mr Justice Hayden, oral judgment)
The ethical and practical dilemma faced by Paul and by the professionals charged with making decisions about his treatment is not unique.
Many people with fluctuating capacity know, when they are well, that they want certain treatments when they are ill – but when they actually become ill, they refuse those treatments. Rather than compel people to have treatments against their wishes, doctors will sometimes accept those treatment refusals. Here’s an example from the Mental Health and Justice Project:
“Many people with Bipolar say that often, when becoming unwell, they lose the ability to recognise that they need treatment or hospital admission. Delays in treatment and/or admission can mean the individual is left to become more unwell and, in many cases, act in a way which is damaging to themselves. An SBD [Self-Binding Directive] is an agreement, written by someone with Bipolar, with the help of their care team and, if they liked, their family/friends. It would explain what usually happens when they become unwell and what sort of treatment is generally helpful. Most importantly, it would aim to make sure that a person receives this treatment, even if they no longer have the ability to recognise that it is needed.[4]”
These ‘self-binding’ advance decisions can include an advance request for coercive treatment in acknowledgement that at the time when the treatment is required (i.e. during an episode of illness) the person is likely to refuse it. The current legal framework in England and Wales makes this difficult to navigate as ‘advance consent’ and so – as in the case described here – the expression of wishes becomes, effectively, an advance statement which contributes to ‘best interests’ decision-making. For one discussion of the form that such a document might take, and how it could work in practice, check out this article about the Preferences and Advance decisions for Crisis and Treatment template. The independent Review of the Mental Health Act also looked at this issue in relation to advance consent for hospital admission (pp. 81-82) and suggested the government should consult about it.
The huge benefit, for people with fluctuating capacity, of making advance statements about their (capacitous) preferences for treatment – knowing that they are likely to refuse that treatment in times of crisis – is that it potentially increases their control and self-determination. Nobody can demand treatment from a doctor who doesn’t think it clinically appropriate and in the patient’s best interests. But where a treatment is the right one and the only obstacle is the patient’s (incapacitous) rejection of it, an advance statement of preferences could increase the likelihood that the person will get the help they know they need and that doctors can act with confidence in treating them contrary to their (non-capacitous) wishes. Having witnessed the distress of the doctor who restrained Paul and gave him treatment against his (non-capacitous) wishes, I think there would also be some comfort for treating teams in having a written statement from the patient that confirms that – despite currently rejecting treatment – the person would give consent to the treatment if they had capacity so to do.
For Paul, the outcome was the one he wanted – at least at time of capacity. In that sense it was an enhancement of his autonomy. But it fell short of granting him the autonomy to consent to treatment in advance of losing capacity. It was not up to him to consent in advance to treatment. That decision was not his. it was a best interests decision made by the court.
Celia Kitzinger is co-founder and co-director (with Gill Loomes-Quinn) of the Open Justice Court of Protection Project. She tweets @kitzingercelia
Photo by Karsten Winegeart on Unsplash
[1] All quotations are as accurate as I can make them given that they are hastily typed out during the hearing itself and hearings cannot be audio-recorded. They are unlikely to be word-perfect.
[2] This was described by counsel appointed by the Official Solicitor as a “somewhat uncomfortable” position since apparently Paul does have litigation capacity.
[3] Prior to the August application, the decision to compel treatment via physical and chemical restraint was “made by the clinical team and Paul’s father”, according to counsel for the hospital Trust. Mr Justice Hayden expressed surprise (“I raise an eyebrow at that”) and pointed out that he had issued guidance in January 2020 and it is “difficult to see how the pre-August treatment followed that guidance”. Indeed.
[4] The work draws upon this earlier work by Tania Gergel and Gareth Owen which can be downloaded as a pdf (click here)